Drug development timeline acceleration strategies for clinical operations

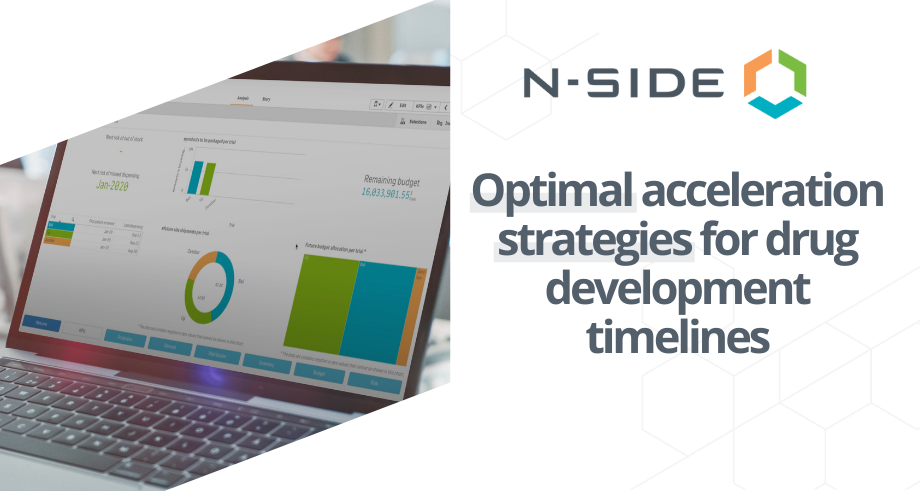
It’s no secret that clinical trial timelines are getting longer. As trials become more global and protocols and therapeutics become more complex, clinical research is simply taking more time than it used to.
Despite this reality, sponsors are under pressure to decrease the timeline and costs of drug development.
At N-SIDE, we work with leading life science companies to streamline the clinical trial supply chain. Through these collaborations, we’ve been able to see how the industry’s top-performing teams speed up drug development timelines while reducing costs.
In this article, we’ll assess some of the most important bottlenecks that delay clinical research, and detail strategies that Clinical Supply, CMC, and ClinOps teams can use to break through them.
For an even more detailed look at how these strategies accelerate time to market, download the whitepaper.
Common bottlenecks extending drug development timelines
There are hundreds of reasons why clinical trials today take longer on average than they used to. At N-SIDE, we focus on understanding and alleviating bottlenecks in the clinical trial supply chain.
Some of the most common supply chain bottlenecks affecting clinical research are:
Drug availability — Every site needs a certain amount of drug to meet expected demand, plus overage to cover demand variability. Limited drug availability means fewer sites and depots can be opened and fewer patients can be enrolled, leading to longer timelines. This bottleneck is even more pronounced in cell and gene therapies, for which drug availability relies on the capacity to collect cells from safe donors.
Allocation issues — Sometimes availability isn’t the bottleneck, but rather how those drugs are distributed to different trials, depots, and sites. Non-optimal allocation leads to some trials getting more than they need (which might expire or otherwise be wasted) and some getting less than they need (meaning they can serve fewer patients and the trial moves more slowly).
Manufacturing capacity — If there isn’t enough drug product, the best thing to do is make more. Unfortunately, manufacturing often acts as the bottleneck, with limited capacity with which to increase production. Both in-house manufacturing and CMO resources are typically booked months in advance, with little flexibility for last-minute changes.
Comparator sourcing — More and more trials are relying on comparators which are difficult to source, slow to produce, and often have limited shelf life. Bottlenecks in comparator sourcing are particularly tricky because in most cases there’s very little a sponsor can do to acquire more.
Budget — In some cases, it’s not manufacturing capacity or comparator availability that’s acting as a bottleneck, but budget. Annual budgets are based on expected demand and usually can’t support unplanned lots. When there are limited funds, teams can’t produce or source the additional drug that would enable them to speed up the trial process.
Siloed data — Though you might not think of data as a part of the supply chain, a lack of shared data between teams can be just as much of a bottleneck as supply or manufacturing. Without shared real-time data, making optimal decisions becomes much more difficult and time-consuming. Siloed data often leads to unnecessarily duplicated buffers at different stages of the supply chain managed by different persons or departments. These unnecessary buffers further increase losses and, in turn, put more strain on the supply chain.
Clinical trial strategies for timeline acceleration
How can sponsors break through these bottlenecks and speed up trial timelines? There are a few proven methods, each involving different teams and relying on enhanced collaboration between them.
1. Improve demand forecasts to reduce overage.
When availability of drug product is a bottleneck, the usual course of action is to slow down the trial (opening fewer sites and enrolling fewer patients). However, clinical supply teams have another option available to them: reducing overage levels.
Because most clinical trial forecasting tools only predict average demand, safety buffers to reduce the risk of a stockout are usually calculated as rough estimates, and therefore are typically very high, and sometimes redundant. In an average trial 55-75% of drugs are wasted.
Using risk-based clinical trial supply optimization to simulate trial demand and model uncertain parameters, clinical supply teams can understand required overage based on minimum and maximum demand levels, and supply only as much extra drug as is needed to each country, depot, and site to cover real uncertainty in the forecast. This applies to comparator sourcing as well. Clinical supply teams can also use this approach to adjust the overage with confidence as the trial progresses since uncertainty decreases as more patients are randomized.
Reducing required overage enables sponsors to open more sites, recruit more patients, and speed up research without any change in the total amount of drug product available. In some cases, reducing overage can even make it possible to accelerate the start of another study, taking advantage of the still usable remaining drug product.
2. Model different production scenarios.
Increasing production capacity isn’t the only way to address limited drug availability. Sometimes, optimizing various production parameters can get more drugs to more trials and sites without adding additional manufacturing resources.
By testing different scenarios involving parameters such as lot pooling, lot sizing, outsourcing, and stability planning, bottlenecks in this part of the supply chain can be alleviated.
Cutting-edge software enables CMC teams to model changes to production parameters and predict the effects these changes will have on supply.
3. Optimize allocation.
By reducing required overage and optimizing production, more drug product becomes available for the trial. This has impacts further up the supply chain as well, as more drug substance and drug product will be available for all trials in the program.
By breaking down data silos and providing a single source of truth to stakeholders at all levels of the supply chain, optimal decisions regarding the allocation of resources to different trials, depots, and sites can be made. Solutions like the N-SIDE, which enable real-time data sharing and collaboration between teams, give CMC teams the ability to make data-driven decisions about allocation.
Unlocking end-to-end optimization
N-SIDE has helped optimize over 10,000 clinical trials to proactively mitigate risks and curb drug waste. Learn more about how you can achieve end-to-end optimization of your clinical trial supply chain in this whitepaper:
End-to-end clinical supply chain optimization helps bring drugs to market faster.



About the Author
Passionate about problems solving and supply chain, Chloé started her journey at N-SIDE by working on the supply optimization of numerous clinical trials. She is now focusing on clinical manufacturing optimization for both large pharma companies and biotechs. This experience allows her to provide robust manufacturing and packaging plans while reducing waste and costs at program level.
Chloé Delhaye



Article
Forecasting and optimization in clinical trials
Learn about the latest advances in clinical trial forecasting and optimization. Understand how technology can help you overcome challenges you face in your clinical trial supply management.
Read now
White paper
Accelerating time to market
Hear from Biotech industry experts how challenges in clinical trial supply and manufacturing can be overcome with innovative software solutions.
Discover more
Article
Enable faster clinical trial timelines through an optimal supply chain
Waste reduction has been identified has one of the causes of slower clinical trials timelines. However, whereas waste reduction is often coupled with cost reduction, wasted drugs, when allocated efficiently, can also be enablers of faster timelines.
Read now


