IRT optimization in clinical trials: achieving maximum efficiency

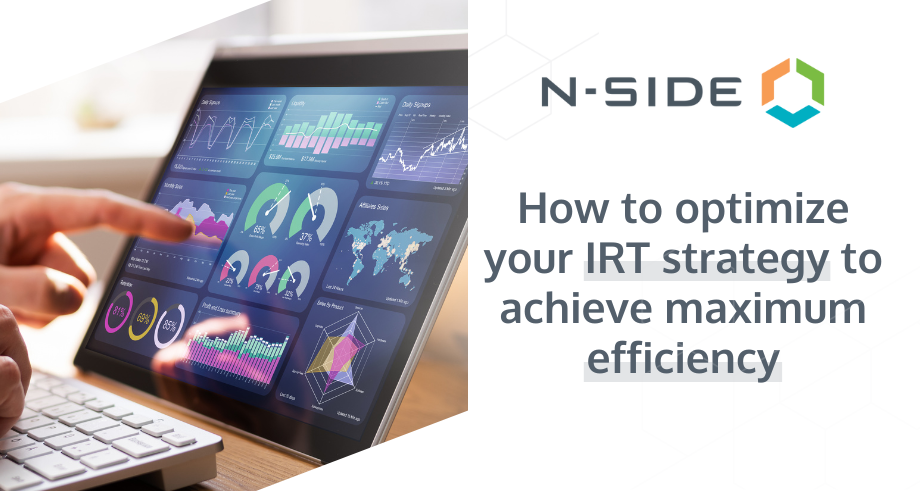
Clinical trial supply managers work hard to ensure trial protocols, supply plans, and resupply strategies are designed for maximum efficiency.
But there’s another way to improve efficiency that’s often overlooked: optimizing the IRT strategy.
Did you choose the best IRT system for your trial? Is it set up in a way that enables an optimal supply plan?
By optimizing the IRT strategy, supply managers can reduce drug waste and associated costs and delays while also reducing the risk of stockouts.
Here’s how:
Choosing the best IRT system for your clinical trial
Optimizing your IRT strategy starts with choosing the right system. Different systems provide different capabilities, and some are more flexible than others.
At the same time, not all trials require the capabilities of the most advanced IRT systems.
When choosing an IRT system, start with a solid understanding of the specific supply needs of your trial. Then look out for the following capabilities:
Flexibility for different usability periods
Does your trial require a combination of drug delivery rules with different usability periods, e.g., an injection that’s valid for one day and pills that are valid until the next visit?
Not every IRT system supports this level of complexity. Being able to manage expiration dates and define the Do Not Ship (DNS), Do Not Count (DNC), or Do Not Dispense (DND) days based on different usability periods provides more flexibility and helps prevent valid kits from being wasted.
Smart prediction (aka randomization prediction)
Smart prediction (also called randomization prediction) refers to a feature offered by some IRT systems that uses a predictive algorithm to send the right quantity of kits to sites only when those kits are needed. In other words, if there are no patients being screened, the kits are not sent, which prevents sites from being overloaded with safety buffers that could potentially be wasted.
Unlike static safety buffers, smart prediction manages stock automatically based on the patients being screened. It’s a lower-stress strategy for trial managers, who don’t need to track buffer levels at the site level or update them manually at any point.
However, smart prediction can only be implemented in some trials depending on the study design (namely the screening period and shipping lead time). The decision to use smart prediction should be based on the best trade-off between shipping and material costs.
Dynamic buffers
Similarly, some IRT systems have the ability to adjust buffers as the trial progresses and evolves.
IRT systems with dynamic buffers activate safety buffer shipments based on specific triggers. These triggers can be set up in a way that prevents the system from sending too much drug to each site.
Other considerations
If technical capabilities were all you had to consider when choosing an IRT system, the best advice would be to choose the most advanced solution available. However, there are other considerations to keep in mind.
Cost is a primary consideration. Generally, more advanced capabilities mean a higher total cost. But don’t forget that a less expensive system might actually cost more in the long run if it prevents you from implementing an optimal supply strategy.
Setup time should also be considered. With trials taking longer on average, adding a month or two to the start of a trial timeline for IRT setup can have a major impact. Conversely, choosing a system that you’re more familiar with or that has a shorter setup process can help accelerate the trial.
Using data to choose an IRT system
It can be helpful to take a data-driven approach to choose an IRT system. Solutions such as the N-SIDE Supply App enable clinical trial supply managers to simulate how different IRT systems’ capabilities will impact their supply strategy.
Benefits of optimizing IRT settings
Once you’ve selected an IRT system that meets the unique needs of your trial, it’s time to optimize the IRT settings to ensure you get the most from that system.
IRT settings categories that should be optimized include:
- Buffer/safety stock levels (to cover unpredictable demand)
- Site shipment frequency (to cover predictable demand)
What does it mean to optimize these settings? Firstly, it means defining a safe strategy that eliminates the risk of missed visits due to stockouts while balancing material and shipping costs.
It also means using the IRT to set the right quantity and shipment frequency to reduce waste and costs to the lowest possible levels without increasing risk.
Finally, it means aligning the IRT settings with the supply plan and depot resupply strategy to avoid unplanned variations in quantities released, shipped to depots, and shipped to sites.
Read more: What is clinical trial supply optimization?
When site shipping frequency and buffer levels are optimized, you can:
Reduce risk to patients
Reducing safety buffers used to mean reducing safety. But with a risk-based approach, you can set up the IRT to avoid sending too little drug to sites or emptying your depot faster than necessary. By creating a supply strategy that accounts for uncertainty in demand forecasts and aligning the IRT settings with this strategy, you can define the optimal buffer level without increasing the risk of patients missing doses.
Reduce drug waste
By sending only as much drug to sites as is needed to cover patient dispensing using a risk-based approach, you can reduce the total drug needed for the trial. This in turn significantly reduces costs.
Reduce stress for the trial team
When the IRT settings and supply plan are in perfect alignment and both are optimized using a risk-based approach that evolves as the trial progresses, it creates a more robust, more flexible, and safer trial with fewer emergencies for the team to handle.
N-SIDE’s solution: Risk-based optimization
As described above, a risk-based approach to clinical supply optimization is the key to optimizing the IRT system and achieving maximum efficiency. But what does this mean?
Risk-based optimization is a technique enabled by advanced software and expert services. Currently, this solution is only offered by N-SIDE.
Unlike clinical supply forecasting tools which only predict average demand, risk-based optimization uses simulations to anticipate uncertainty and risk to the trial supply.
With this information in hand, clinical trial supply managers can depend on a supply plan and resupply strategy that includes the lowest amount of drug overage necessary to guarantee zero risk of a stockout.
N-SIDE is not a provider of IRT software. However, the outputs of the N-SIDE Supply App do help clinical trial supply managers choose the best IRT system for their trial. Outputs of the N-SIDE Supply App are also used to set site shipping frequency and buffer levels.
Additionally, the N-SIDE Supply App integrates with most IRT systems, enabling supply managers to compare the actual data coming from the IRT with the clinical assumptions used in forecasts as the trial progresses.



About the Author
Jonathan joined N-SIDE a few years ago as a consultant in the Life Sciences Department. Passionate in the more technical aspects of the work, he switched to the Life Sciences Product Department in order to work on the software and its applications. He recently came back to LSD as head of a team focusing on technical expertise, including IRT integrations.
Jonathan Dehaye



Content that might interest you

N-SIDE Supply App
The N-SIDE Supply App is the only solution that adds a risk-based optimization approach to clinical supply forecasting.
Make data-driven decisions about overage, packaging, sourcing, IRT setup, depot shipments, and more, all while measuring the precise impact of these decisions on patient service level and budgets.
Webinar
Understanding the benefits of risk-based optimization on clinical trial supply planning
Learn how to identify the differences between risk-based optimization and forecasting for clinical supply chain and manufacturing planning and much more!
Watch now
Article
Take the guesswork out of clinical trial supply overage
With risk-based optimization, Clinical Supply Managers are able to manage their trials in a more relaxed and efficient way, without worrying about having enough overage.
Read now

